Space Summary
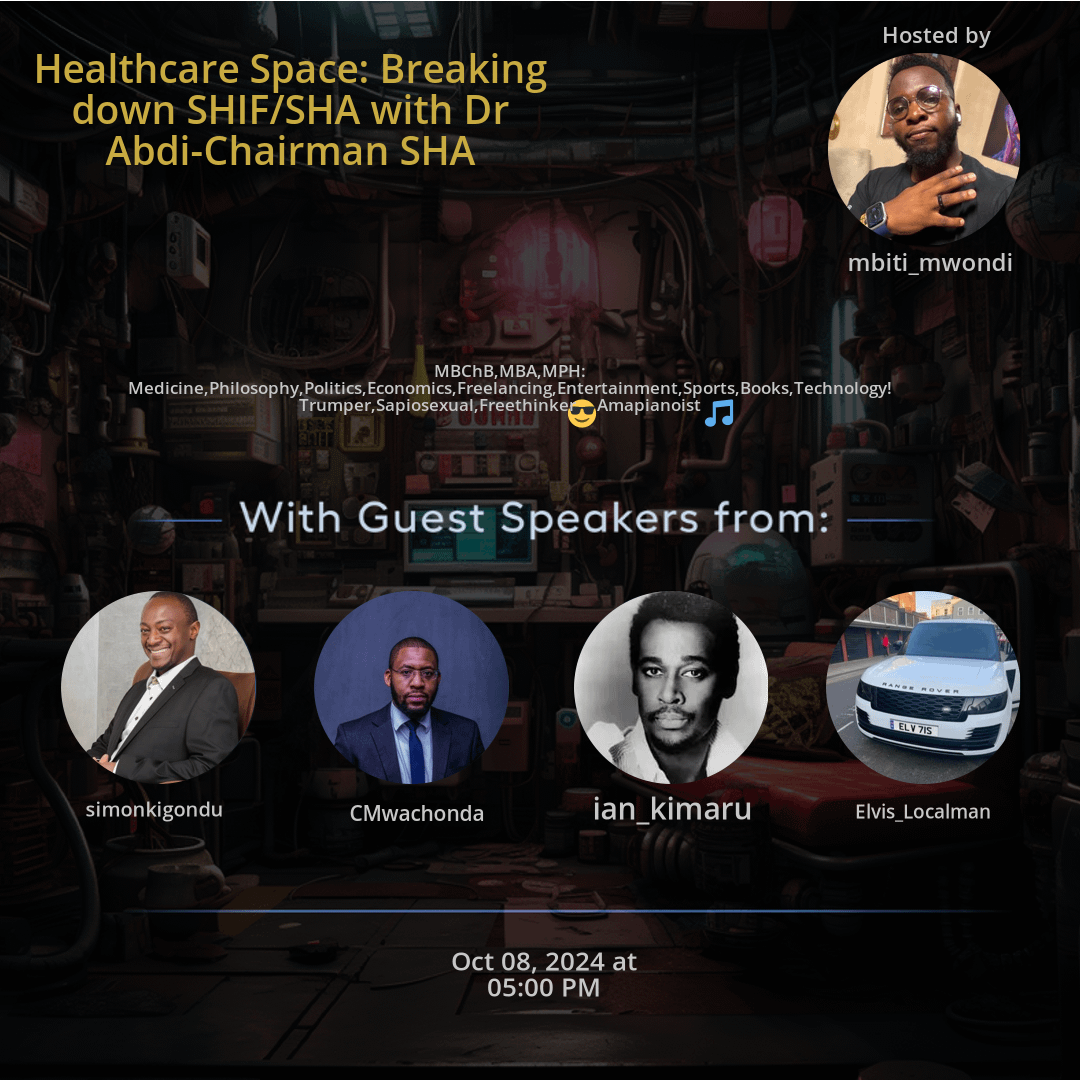
The Twitter Space Healthcare Space: Breaking down SHIF/SHA with Dr Abdi-Chairman SHA hosted by mbiti_mwondi. Delve into the diverse world of healthcare with Dr. Abdi as he shares insights from various fields like medicine, philosophy, politics, economics, and technology. Explore the multifaceted aspects of his personality, from being a Trumper to his passion for Amapianoist music. With discussions ranging from entertainment to sports, books, and technology, this healthcare space offers a unique blend of topics that showcase the broader landscape of well-being.
For more spaces, visit the Unique Projects page.
Space Statistics
For more stats visit the full Live report
Questions
Q: What fields does Dr. Abdi specialize in?
A: Dr. Abdi brings expertise in medicine, philosophy, politics, economics, and technology to the healthcare space.
Q: How does Dr. Abdi's diverse interests contribute to the discussions?
A: Dr. Abdi's diverse passions in freelancing, entertainment, sports, books, and technology enrich the healthcare space.
Q: What personality traits define Dr. Abdi?
A: Dr. Abdi showcases traits like being a Trumper, Sapiosexual, and Freethinker in the discussions.
Q: Why is music mentioned in the space description?
A: Music is part of Dr. Abdi's interests, especially his passion for Amapianoist, providing a glimpse into his multifaceted nature.
Q: How wide is the range of topics discussed in the healthcare space?
A: The discussions cover various aspects ranging from medical practices to lifestyle topics, showcasing the diversity of content.
Q: How does Dr. Abdi's background contribute to the depth of discussions?
A: Dr. Abdi's background in multiple fields adds depth and richness to the healthcare space conversations, offering diverse perspectives.
Q: What makes Dr. Abdi's participation unique in the space?
A: Dr. Abdi's unique combination of expertise and interests makes his contributions special, enriching the healthcare discussions.
Q: Why is technology relevant in the healthcare context?
A: Technology plays a crucial role in modern healthcare, influencing practices, research, and patient care.
Q: How do diverse interests contribute to a broader understanding of healthcare?
A: Exploring diverse interests like sports, books, and entertainment alongside healthcare provides a holistic view of well-being and lifestyle.
Q: What role do personal traits play in healthcare discussions?
A: Personal traits like being a Trumper, Sapiosexual, and Freethinker add personal perspectives and uniqueness to the healthcare space interactions.
Highlights
Time: 00:15:43
Diverse Expertise in Healthcare Dr. Abdi's vast knowledge in medicine, philosophy, politics, economics, and technology.
Time: 00:25:18
Passion for Amapianoist Exploring Dr. Abdi's love for music and his involvement in Amapianoist.
Time: 00:35:52
Discussion on Personal Traits Insights into Dr. Abdi's unique traits like being a Trumper, Sapiosexual, and Freethinker.
Time: 00:45:36
Incorporating Entertainment and Sports Exploring the blend of healthcare discussions with entertainment and sports interests.
Time: 00:55:21
Technological Impact on Healthcare Insights into how technology influences and shapes modern healthcare practices.
Time: 01:05:47
The Importance of Philosophy in Medicine Discussing the role of philosophy in shaping medical ethics and decision-making in healthcare.
Time: 01:15:12
Economic Considerations in Healthcare Exploring the economic aspects and implications in the healthcare industry.
Time: 01:25:59
Freethinking in Healthcare Discussions How a mindset of freethinking influences innovative healthcare approaches and discussions.
Time: 01:35:28
Book Insights in the Healthcare Space The relevance of literature and books in expanding knowledge and perspectives within healthcare.
Time: 01:45:03
Bringing Politics into the Healthcare Conversation Understanding the intersection of politics and healthcare policies in the discussions.
Key Takeaways
- Understanding the intersection of medicine, philosophy, politics, economics, and technology in healthcare.
- Insights into the diverse interests and expertise of Dr. Abdi, including freelancing, entertainment, sports, books, and technology.
- Exploring the multifaceted nature of individuals like Dr. Abdi, who embrace a wide range of passions and professions.
- Insight into the personality traits of Dr. Abdi, including being a Trumper, Sapiosexual, and Freethinker.
- Exploring the connection between music and Dr. Abdi's passion for Amapianoist.
- Insights into the broad spectrum of topics covered in the healthcare space, from medical practice to lifestyle interests.
Behind the Mic
Introduction to the Healthcare Space
It. Yeah. Nigel. Am I audible? Nicole? Yeah. Nakuskia. Yeah. Okay, nice. Yeah. So, good evening, guys. Welcome. Welcome to a space we do have sometimes. I do host healthcare spaces. We have discussed matters, the issues that we face in healthcare. I think I've talked about last time I had held a space on matters healthcare, were talking about the interns issues, I think after our colleague had died by suicide. We're discussing about the issues that we face in healthcare. At that point was matters, interns, HR issues, working conditions, toxic employers and all those kind of things. This is the second. This is now the subsequent space. We want to talk about healthcare. It's an interesting conversation because it's a people's space. We have Doctor Abdi Karibu, he's the chairman of Shah. I think he left time to talk to us. And the reason why I held this space is because I also happen to work in a mission hospital and in public healthcare space.
Current Challenges in Healthcare
And we are having a lot of issues. The transition from. From NHIF to Shah as a healthcare provider, also in the business of healthcare, running a clinic here and there. I also have concerns. We also have issues with patients. You know, like the better part of the last two weeks, we have had issues with transitions, the system not working. And also we have the general attitude towards Shah, chief, you know, we have had reject, reject. And this kind of conversations around the new scheme. Of course, there are also questions that regards. There's a lot of money that is going around. You have heard of billions and billions. You've heard of Jayesh, you have heard of so many things that basically has created a certain attitude of perception towards this new scheme. And so that's why I sought for Doc, the chairman, to also come and perhaps raise, or rather give us what. Tell us in detail what this is. Answer some of your questions. And so it's an open space. We'll allow healthcare practitioners, we allow patients to give us the experiences.
Engagement and Respect in the Space
We'll allow people who have opinions on how. I'm sure chairman has. He has been quite consistent and available in trying to raise clarity around this subject. And so ask those questions. I also. My only wish is that even when you are having the conversations, let's be respectful. We are trying to have. We are trying to have answers to what we earn. And also we are trying just to ensure that our healthcare system works, which has been quite a problem with this regime. To be welcome, anyone who wants to speak. It's an open space. It's an open mic. We love doc. Also, tell us about this thing. What questions we have, what concerns we have. I love questions for you. If you have any questions, also you can comment on the space chat. We can pick it up. Any civilian who has a question, who has clarity, who has experiences with the issues that you're facing, you're welcome.
Doctor Nijel Karibu's Input
I have my post. Doctor Nijel Karibu. Give us something before we allow. Doctor, say something, Nija. We have an opening space, or you can have the conversation going. I think what I can say is that this space is actually a nice thing so that you can hear at least now from the chairman himself. So tell us about, especially now, the chief, and so that we can get, maybe get clarity on some of the things that or some of the concerns that we may have about the whole show and shift. Yeah. So thanks. I think I'll give chairman to give us his open remarks. I want him to tell us what this new scheme is, why the government felt the need to change the old system that we had to the new system.
Change in the Healthcare System
Why not have some improvisation on it before we come to what we feel, what we're experiencing in the ground, what our attitudes and opinions are, perhaps what our recommendations also are. Doc Karibu, maybe you can confirm you can hear us and you can say something. Yes, I can hear you loud and clear. Thank you very much, Madaktari colleagues, my junior colleagues, when you requested, I told you I'm ready and available to clarify the issues. The reason is because there has been a lot of misinformation that has been going on, and I understand because generally, trust is an issue that we have had. So on that note, I thought it would be wise for me to just come in and explain some of the issues which are clearly not true, and then just lay bare what is the whole idea. So I think people are aware that there were four laws that were passed, the UHC laws, October 19, 2023.
Overview of the New Laws
So the four laws, if you look at them, there is first one, which is the facility improvement fund. The second one is the primary Health Care act. The third one is the Digital Health act. The fourth one is the Social Health Insurance act. So I will just try to explain briefly what each one is meant to do. So the f. The Facility Improvement act was meant to ring fence healthcare money to the facilities. Currently, as it is, some counties have that law. Some don't have. Some counties allow 30% of the money to remain in the facility. Others 50, others 70, others 80, some a few 100%. So what we wanted to do is when facilities collect money from user fees or from NHIF or from whoever is paying, whether it's private insurance, they use that money to improve the facilities. And I'm talking about public facilities, so that money is reinvested for health.
Financial Management and Public Participation
So the idea of a facility generating, let's say, 100 million, and then it gives to the county government, it goes to the county, then it's the mcas that decide how that money is going to be used, which sometimes they receive 20 million back or they receive nothing back, and that money is used for other purposes. For that reason, we said, lets have a law that makes it mandatory for all facilities to keep their money. So the law was passed in Senate, so that is mandatory now to all facilities. So the second thing is the public now, just to make sure that they participate in running those facilities. The act also allows the community to be part of the health management team for level two and three. They sit and it has youth representative, it has women, it has like almost six seats are reserved for the community in the health management board for those facilities, level two and three, and level four, five, I think they have one seat or something to that effect.
Implementation of Healthcare Improvements
So this is meant to keep money in healthcare. Budgetary allocation plus collection remains in the facility. There should be no excuse that the facility doesn't have healthcare workers, or no excuse for the facility not having money to buy drugs. Second act was the primary healthcare act, which now introduces the issue of community health promoters. Previously, these guys were there, but they were run by NGO's, and they used to do small in a county, they would go to one ward and then they are paid a certain amount. They do one condition and they carry big registries, books to record for one disease. So they were doing one activity in one place and nothing else. And guys used to collect millions of dollars outside Kenya in the name of community health.
Reforming Community Health Initiatives
So what we thought is the national government should be able to pay stipend to these people and have across all the 47 counties, across all the wards, and then give them phones digitally to be able that registry instead of doing it manually. They collect the data through the phone. And there is an electronic community health information system that allows for them to record the necessary inputs. So some of the things that they find out is whether the children are malnourished. So they do tape measure to measure the babies. They look at whether they are pregnant mothers. They ask whether they have gone for the clinic, ANC. If they have not, they encourage them and link them to the nearest facility to go for the clinic to start. Then if they find people who have chronic conditions, hypertension diabetes.
Essential Community Health Functions
They do run of blood sugar, just to check whether they are properly controlled. If not, they tell them to go to the facility. So their work is basically to assess and link. That's it. They don't treat anyone. They just make sure they educate the mothers on wash in terms of the usual hand hygiene and all those things. So that the mothers understand on how to do prevention. So they are more on prevention and linkage to the facilities rather than treatment. Then the third act is the digital health. So the challenge we have had is we have paper. You cant run. On pieces of paper. Its impossible to have silos. Data is in different systems, in different books, in different registries. So the ministry is not able to plan.
Digital Infrastructure for Healthcare
The county is not able to plan, because we don't know our disease burden, how big it is. We have had what we call Kenya Demographic health survey, which happens every ten years. So every ten years means one government starts its term and then the assessment is done when it's exiting. So that government has no information on how utilization, ANC coverage, family planning, skill delivery for mothers. They don't have all that information. That information comes out after ten years. So new government finds the scorecard of the previous government. Then they remain in the dark for ten years. When they are exiting is there will be another scorecard. So because of such things, and because of duplications and data, which you don't have a way to provide policy direction, where do you need to invest?
Addressing Inconsistencies in Healthcare Data
How much do you need to invest? We have never known, because of the manual system that we are operating on, and the silos. So you will find a patient walks into this facility, they walk back to the nearest facility. That patient repeats all the tests because he hasn't carried his results. So the other hospital says, we don't know whether you have been tested or not. So we are repeating the tests for that reason we said, and the Health act of 2017 also says the same, digitalize and connect. So now what we are doing is connecting all public health facilities, all private facilities, all pharmacy outlets and standalone laboratories. And then you have client registry, you have facility registry, which has a single source of truth.
Challenges with Medical Supply Authenticity
Then you have all healthcare workers. So we have a lot of quirks in the health industry. Unfortunately that is, people take advantage. And then we have a lot of healthcare workers who are unemployed. So you have mismatch. There are quirks in the system who are operating nicely, making money. Then you have young skilled workers who have gone through the system and licensed, not getting jobs. So now you cannot be able to work and see patients. If you are not licensed, because it's the license number that you will use to see patients and registry, then the other thing is, we have a lot of fake drugs in the country through whichever routes that they come in. Unfortunately, there is no one who does track and trace.
Addressing Forged Medications and Prescription Issues
We are not able to know this medicine. Where did it come from? From which country? Who is the manufacturer? Who is the guy who imported it in? Who is the distributor? Which facility has it gone to? Which patient has been prescribed for? Thirdly, there is a lot of misuse of antibiotics. Patients are just walking into a pharmacy with no prescription, asking for certain drugs, and they are given. So misuse of antibiotics, misuse of codeine and such controlled drugs, because there is no one who is looking at the prescription, because everything is manual. And that's the reason why we said that is impossible to run UHC on that kind of paper based system.
The Goals of the Digital Health Act
So that's the essence of the digital health in terms of what the gaps it's trying to address. I think was it some time back I saw a study that came out. It said out of the 17 syntosin on drugs that they have sampled, for those who are not medics, synthosinone is the medicine that we use to stop mothers from bleeding when they deliver, so that they don't get postpartum hemorrhage. They don't get bleeding after they have delivered. They said only six had active ingredients. Eleven were useless. In terms of the content, in terms of the input, the ingredients, there was no active substance. So that tells you a lot the problems that we are facing, because there is so much fake, and then because you have picked that sample from the market, you are not able to trace back to where it came from, because you will find whatever number that is on the vial, because you don't know originally where it came from.
Concerns Regarding Medication Quality
When you go back to the manufacturer and say this is your drug, they will tell you, no, no, this is not our batch. We don't know where it came from. So because you don't have any evidence contrary to it, you are just stuck. So for that reason, we have the track and trace as part of the digitization. Finally, we have the big elephant, the Social Health Insurance act. So the Social Health Insurance act is meant to change and replace Nhif. I see a lot of people saying reform, but when you look at the dictionary, the meaning of reform, it's exactly what we have done. You change the structure, the process of something. That's how you reform NHIF act has been amended I think almost four times since it started and we have done a lot of changes to it to the point that now amending it further will not make any sense.
New Structures within the Healthcare System
Plus, the new Social Health Insurance act is meant for everybody, while NHIF was meant for members. So the difference is there are benefits that you can get from NHIFDev only if you are registered paid up member. While for Shah you have. We have introduced three funds. So the first fund is primary healthcare fund. The second fund is shIf, which now is comparable to the NHIF because that one you need to be registered contributor for you to benefit. So those two are equal, shif and Nhif. But remember, under Shah you have primary healthcare fund and then finally you have emergency chronic critical illness fund. So primary and emergency chronic critical illness fund are two funds that are appropriated by parliament.
Budgetary Allocations and Fund Management
And the money comes from treasury. So it's taxpayers money. So this is one area that you can lobby and push your member of parliament to allocate resources because you benefit it just by being a Kenyan without even contributing for NHIF. That was not possible under Nhifdev. So what else have we done that makes it different that people are wondering why have we not reformed and not. So the other thing that we have done is we have created a board membership that incorporates everyone. For the first time, we have the director general sitting at the board of Shah in NHIF. He was not there. He was not part of the Nhif board.
Enhanced Representation and Accountability
For the first time we have informal sector representative. So they have a seat. Previously it was occupied. That seat was left for the Federation of Kenya Employers. But we said the majority of the contributors will be the hustlers. They deserve a seat rather than FKE. So that seat is given to boda association, stroke, Juwakali and Matatu. So it will be sort of rotating amongst those three major associations. Then the other thing that we have made a change is who represents the counties. So previously it was the secretariat for two seats. Now we changed. We said one is the secretariat, but the other one is the other one. We will leave it to the CECs because they are the ones in charge of health and they are the ones who understand the problems that they face.
Transforming the Structure of Healthcare Governance
So they should be seated on the table. Then the other thing that we said is the providers private admission also need a seat. Then Kenya Medical association to represent the healthcare professionals to have a seat. That is the governance in terms of. And then the workers, of course, the unions represented by court. So after that, now the next thing that we have done is to say what else was the challenge. So the second challenge was NHIF used to operate on paper based. So we said the process for SHA needs to be digitized from end to end. Then what was the other problem? NHIF used to have an open check in terms of how much can they use for administration?
Operational Efficiency and Accountability
Administration means they can buy cars, salaries, travel per diem, buy computers, paper, do road shows, all those things, allowances. So they had an open check. So what used to happen is at one point it was 80%, they will consume 80%. It came down to 50, it came down to 30. The latest was 15%. So 15% of everything that they collect was used for administration. But for Shah, we said that's too much. Industry practice at best is usually 5%. Why should a government body not conform with industry practice, which is the best practice that is well known? So we said, for that reason, let's put that thing in the law, so that it's not dependent on the goodness and the willingness of the board and management.
Regulatory Changes for Transparency
So it's in the act. Administrative cost cannot go beyond 5%. Maximum 5%. It can be lower, but it can't go beyond 5%. Then we asked ourselves, what was the other issue? So if you're a healthcare provider, you know, if you wanted to be onboarded by NHIF, you needed a lot of talking to brands to, I don't know who wait for the board to gazette you. And that used to take almost a year or two. If you are a provider, you know, a year or two, and that is the empanelling. But what has Shah done? Shah has said no empanelling should be done by the regulator who licenses facilities. They are the ones who know whether my facility is licensed or not.
Streamlining the Onboarding Process
So they give us the list. Once they license you and they give us the list, we empanel you within 30 days. We don't wait for, by law, within 30 days, we empanel you. Secondly, for this one, we have even removed the empanelling within 30 days. We now, we are doing it now real time because we have connected to their system, which is their registry. So if you are in panel today, if you are licensed today by the KMPDC tomorrow, you appear on our list automatically because we are connected to them directly. Then the second thing which has delayed is the e contracting. So as a facility now you can proceed and say you can find yourself, you have been licensed, you move to the e contracting portal, you start contracting, you apply and say, I am ready to offer the services, and you fill in your details, and you sign the contract and you send it back.
Enhancing Efficiency with E-Contracting
So how are we able to do that part? Because the reason why were able to do that is the prices, which is the benefits, and the tariffs is something that we have also gazetted. So those two benefits and tariffs undergo public participation, providers, professionals, patients. That is the process it undergoes. When we are finally done, it's gazetted. So if you google today, benefits and tariffs, for sure, you will find in the gazette notice and you will see what benefit you are entitled to and what tariff you are entitled to. So that makes it easier to contract the facility because the facility can already see these are the prices and these are the benefits.
Continuous Assessment of Healthcare Services
And for me, these are the services that I have. I can provide services based on this. But more importantly, because we know those benefit and tariff is a live document. It's a document that needs to undergo changes, because things change every now and then. The disease burden change, the money that you collect changes, the incidences change, the cost of doing business change. So you need to update regularly. So for that reason, in the regulations, if you look at it, we have created a committee of around, I think 1112 people. It has representative from Shah, it has representatives from the Ministry of health, it's based at a university for purposes of doing that research and coming up with a proper costing.
Stakeholder Engagement and Representation
It has a representative of patients, it has a representative of providers, it has experts from actuarialists, health economists and epidemiologists. So that committee can be petitioned by an individual, by an association, by providers, and say, we think the price of this is too low, or you can go and say you have forgotten to cover this disease. We need you to add this disease to the list of benefits. We think the prices of per family is too low. Please increase so they will look at the data, they will look at the information and if you do for them the data and the analysis and the burden, even better, because you will go with evidence.
Promoting Transparency and Participatory Governance
It is not just a request. But more importantly now you can also petition your parliamentarians MP's to say, because chronic conditions x we want you to allocate more money from the budget during the appropriation. So that also now makes it transparent. NHI have never had these things. All the things that I've mentioned so far were non existent. The benefits and the tariffs, no one knew. It's only the provider who knew. The patients never knew how to amend and how to change the. It was just NHIF on its own who was participating. They were doing it themselves and then they were coming and telling us, this is what we have decided.
Addressing Dispute Resolution
So that also is something that we have put in place. Finally, we said, because all these things, there will be always challenges in terms of dispute between providers and Shah, between patients and providers, between patient and Shah. We put a dispute resolution mechanism. So we have created a tribunal which is outside Shah and appointed by the judicial service Commission for people and a chair. Their work is to make sure they receive complaints and they are able to sort out and resolve. Previously, that was done internally at NHIF. So NHIF previously was doing the premium. They were deciding how much you will pay.
Transformation of NHIF Roles
Secondly, they were deciding what is the benefits, what is the tariff. They were deciding which provider is on the panel and who is contracted for what rate, because providers had different prices. Anyone who was in the industry knows some providers were paid higher, others were paid lower. Then finally, they were the ones who are deciding if there's a dispute, that they were the ones who are resolving. So if you look at now the act, you will realize that is very much different. And you needed to be a member of NHIF and a contributor for you to benefit. And if you are contributing today, if you are in the informal sector, you are supposed to wait for 60 days before you are getting benefits for sure.
Access to Immediate Healthcare Benefits
So for sure, in terms of patient benefiting for primary healthcare, all you need is just to register. That's it. You don't need to pay anything to benefit because that's tax funding. It's not our money for Shif, which is, for now, the services you will access in level four, five, six, and the primary healthcare is accessed in level two, three. You will have contributed 2.75% of your income. And once you contribute, you benefit immediately. There is no waiting period. You are sick, you happen to be ready today. You just pay and you move on. Not that I am advocating you only pay when you are sick, but there is no waiting period. Finally, emergency care emergency, chronic critical illness fund emergency.
Implementation of Emergency Care Rights
You don't need to be a contributor, neither do you need to be a member. You just benefit because you are involved in an accident or you have an emergency. This one is being implemented now for the first time. Emergency as a right is in the constitution. It has been in the constitution from 20, 10, 14 years down the line. It has never been implemented. It was also in the 2017 Health act. It has never been implemented. This is now the first time we are daring to say we need to give dignity to our people and we need to implement this right. And how are we doing? It's tax funded, so we will not ask you to have registered and to be a paid up member for you to benefit.
Comprehensive Reform Initiatives
So now, I think the listeners now have understood that when they say reform, they can clearly see this reform is not only at higher level, but it's a reform even for the public health facilities through the FIF, the community health, then at the Shah level, through the two primary the primary healthcare fund and the emergency, which now gives access to the poor because they are the ones who are most affected by these problems. Then let me come to the transition, because if I don't speak to it, I will be disingenuous. Has there been a problem? Definitely yes. Could we have done better? Definitely yes. Are there patients who have been affected? Definitely yes. But have we tried to solve all those issues? Yes, one step at a time.
Reflections on Transition Challenges
We have been able to address most of the issues. Most of the challenges that we have faced are now behind us. We have managed to settle a few of the pending problems and hopefully by the end of next weekend, most of the issues that we have faced would be over. So what we will be discussing is how do we now get as many people to pay up as possible? Because the fund becomes only sustainable if many people contribute. It's the issue of the purchasing power. So if we have enough resources, then we are able to say now we can pay providers promptly because we have money. Oh, I forgot one more thing. Nhif was allowed to invest under Shah. We have removed that.
Strategic Financial Management
We said the business of Shah is not to do business. The business of Shah is to pay and finance providers, healthcare providers, public private mission. So you will never hear Shah again. Has bought ten acre of land which has a dispute in Karen. They have built. Shah has built a parking lot that has been in the parliamentary account committee for, I don't know, PIC and PAC for the last 2030 years. We will not, because that's not our business. We have 5% for administration and 95% to pay providers. I think that concludes my just not so brief introduction, which I wanted people to understand first.
Engaging in Open Discussion
Where is all this coming from before? We now delve into answering specific questions. Thank you very much, doc. Thanks, doc. That was exhaustive. One thing, I'm getting a lot of inboxes. This is not a political space. We have not been paid to sanitize anything. I think I actually held this space because I'm a key stakeholder player in healthcare. I'm a doctor, I treat people. I have a clinic. I see patients, like right now, the occupancy where I work, we have an occupancy of 100 bed capacity. And for the last two weeks, you have had four patients in all. No maternity. The whole hospital has four patients, yet it has a capacity of 100.
Healthcare System Transformation
And for that reason there was no way we could have allowed them to remain where they were. Number three, the other question that you have asked was the issue of the system. If you are listening a little bit earlier, you would have realized that, number one, the system is not for sure. The system is digitization, digitalization of the whole healthcare system. And it's not for one entity. Kemsa is in it. Regulators are part of it. All public health facilities, county and national part of it in terms of both hardware and software. And finally, the amount of money is not for one year, it's for ten years. Two years of setting up ten years of this work. So the 104 billion is not for one year, it's for ten years. Finally, I think even the peers talked about this government has not paid a shilling for this 104 billion. Thank you.
Data Privacy Concerns
I can take another set of questions. Let me just rebuttal back a little bit on the second question. The second question. You've said that there was a gazette notice to inform the public that they will be transferring our data from NHIF to shif. But now you see, one thing all of you need to understand is that with things to do with data, I can either say yes or no. And nobody asked me to either say yes or no. So to me, I feel that any data that was moved from NHIF to shif was breached for literally everyone. Because giving a gazette notice or a notice that you're going to move this data from point a to b without consulting anyone, by asking them either to agree or not, that is not how it's supposed to be done. And in my opinion, I think that is a big data breach. And even if you read the GDPRS policies globally, for them to touch any data or come up with a new system and they have to move your information from point a to b, they have to ask you, they send you a text to either you say yes or no. If you say no, they will inquire. They'll try to find out why did you say no? So it can't be just that you come up with a notice and say from date a will be moving information from point a to b and you have to comply. That is not how it works. So that one, I don't agree. Thank you.
Challenges with New Health Initiatives
Thank you, doctor. My name is Gilbert and I work in Ospakot. I'd like to tell doctor one thing. In as much as we are marketing this shift share, let us try as much as possible to be honest to the citizens of this country. When you come and tell us that primary healthcare will be free, it has always been free. There's no one who has been asked to pay for health in our dispensaries and health centers. The only thing that shif is coming to add is that we must now register before we go to those dispensaries and health centers, which I think is an advantage to the majority of Kenyans. Number two, on the issue of dialysis, President Kenyatta did a fantastic job in making sure that many hospitals in the county have dialysis centers. And I've been seeing doctor here and the CS saying that the 10,000 shillings that Kenyans that they shall be paying will cover for erythropoietin and iron sucrose. That will never be enough. 10,000 alone is not enough for consumables for these dialysis in these hospitals and for maternity services. They've also said that it shall be free in our primary healthcare centers. But in levels four and five, I don't know how they'll cater for it.
Concerns Regarding Health Service Fees
So as we speak, hospitals in West Pocot, they are charging mothers to deliver in level four and level. Yeah, level fours, which to me I feel like is taking us back. In the past, NGOs such as Amref have played a big role in making sure that these mothers are delivering in the hospitals. And I feel like these people are taking us back, which we expect to see. The data for mothers delivering in our hospitals really drop if this will continue. And finally, Doctor said that we should wait and see to see that shif will work. So when he says wait and see, what does it mean that Kenyans should suffer more? That Kenyans should die? Like the way there was, that story that we saw in Eldoretz, should we suffer more for them to agree that this thing is not working for all of us? I took my personal, I took my kid to the hospital and I was charged.
Personal Experiences with Healthcare Coverage
I used to get comprehensive cover under NHIF, but right now I'm not getting anything at all. Thank you. Thank you. Let me answer. It's good you talked about comprehensive, and I understand where you are coming from, because people who used to get comprehensive medical cover were the people who work for us, people who are in government, the three arms of government, including national and county government. And that was not sustainable. Actually, that's one of the other main reasons why we had to change and make uniform. In terms of contribution and in terms of benefits, there are no more equal members than others. We are all equal and we should get the same benefits. Secondly, primary healthcare is available in public private mission, it's not in public facilities only. So the capitation is to all the three different ownerships. And if you look at the finance acts of each of the counties they publish, these are public documents. All you need is to look at what are the charges for hospital fees, and you will see it with your own eyes how much it costs to do registration, delivery and all other services that they offer.
Dialysis and Healthcare Funding Issues
That is the finance bills of the counties for you to check. Thirdly, dialysis. What has happened is we have moved it from 9600 to 10,650. I understand when he says that it's not enough. The biggest challenge we have had in this country is we have a lot of brokers in between the manufacturer to the final distributor to the facilities. So even if today we say dialysis will pay 20,000, I assure you the supplier will increase his supplies to 18,000 or 19,000. So the facility will be crying, saying it's not enough, it will never be enough. So we need to find a way of addressing how do we do direct procurement from manufacturers or bulk procurement collectively from one distributor, rather than having 1001 distributors disadvantaging. And there are many providers who are able to provide erythropoietin and ion sucrose. This one I am not talking about from theory. I have done it as a provider when being paid 9600. So it's not hearsay and it's not.
Maternity Services and Health Tariffs
I have been in that position and done it for maternity. Yes, we will pay for both level fours, select level fours and level two and three, and we will pay 10,000 for normal delivery, and we will pay 30,000 for caesarean section. That is what is in the tariff previously, these amounts used to be 2000 505,000. So public facilities now have an advantage. For the first time, we will pay public private mission the same rate. NHIF used to pay a lower amount to public facilities and a higher amount to private facilities. They used to pay 2000 505,000 and they used to pay private facilities 5000 and 17,500 for caesarean, 5000 for normal, 17,500. Those are facts. Unless you can bring different facts, I am willing to challenge anyone to show different amounts than this and to show where public and private were paid the same amount.
Equity in Healthcare Payments
It's the first time and it's a public document. Go. And Google benefits and tariffs, you will see it doesn't differentiate the ownership of the facility. Prices are the same. Thank you. But I'll give you a chance to comment. Darwin and then Darwin and then Mohammed, and then Doctor Mbiti. Thank you very much. I don't know if I'm audible and clear. Yeah, yeah, go ahead. Thank you, doctor Abdi. Thank you. I've been listening. And first of all, let me just declare my stand. I have never supported this shifting. Because. Of some very many reasons. In as much as I've tried to flip it and look at the good side of it's still not appealing. So let me start here, because I work in the hospital. I wake up to go to the.
Observations from Healthcare Professionals
Hospital to deal with patients, go back, and that is my day to day routine. And the fact of the matter is, there is suffering. The suffering that is going on. In. The spaces of hospitals is so despicable. You know, there is nothing, there is no media that can report the amount of tears which are not focused on camera friends. And Doctor Abdi, there is so much suffering. I work in the surgical unit. I have cancelled lists because of NHIF and shutting the program. The thing of Shah, it's just not working. And you see, I don't know. You know, when I listen to you speak, I hear very good English verbs and very good promissory talks, which are very sounding to the ear. But you see, where I work and the spaces I feed on to the colleagues who are in these spaces, people working in private facilities, there is suffering that even if Shah starts working now, Shah will never pay the losses and the pains that citizens have inflicted themselves because of this unturned and unsaid delays.
Critique of Healthcare System Transition
So one, you rolled out a system which was not pretested. And now the rolling out of the system came with a lot of political language, also to Shiv, because Shif is coming to take a lot of my money, it's coming to give me services that are not equated to the money, and it's going to be privatized and run by some individual. So, first, there is no political acceptance of this shift. Two, there's someone who's advising the CES and the Ministry of health where you sit, and they are not telling you the truth. So my brother Abdi, the chair, the suffering that the people are going through, you may not compensate the losses. Some people, you know, when you speak about dialysis and missing a session, it may look very easy, but it is very difficult because these people depend solely on those dialyzing machines. I've heard you say, wait and see. We can't wait anymore. We can't see anything right now.
Concerns About Indigence Identification
There is no formula. There is nothing to show that this is a person who is an indigent. So you will find when you run that data, the chief has put his wife as an indigenous. Surely, how can your wife be an indigenous and you work for government? It loses the meaning of who is an indigenous. So how are we doing it? We are not deploying money to collect that data to identify indigenous. The proximity testing is something that you do from your phone. You just go to Afeyangu portal, you register, you fill in, you answer questions, and you will be able to get, if you are an indigen or not, it will tell you if you get a payment of 50 shillings and below as your premium, it means below 300 shillings, then it means you are an indigent and you need to be paid for. So there is nowhere you are embarrassing yourself to say, identifying yourself, you are doing from the comfort of your home.
A Clear System for Indigence Identification
There's no one who is coming to tell you are an indigent. And that means you are automatically paid for. And when you go to a hospital, it just says you are eligible. It doesn't say you are an indigenous. There's nowhere it's mentioned that you have been paid for. It says you are paid up member and you benefit. So there is no money and there are no enumerators that we are sending to the field to go and identify indigenous. So there is no cost. Two, that is data that we have trained and modeled. And this is data that was done by the Kenyan National Bureau of Statistics. The survey that they did for poverty is the one that we have used as the base. But we also did for eight counties. We went and tested the data and modified to make sure that what it brings out, it rather underestimates than overestimates.
Testing the Effectiveness of Data Collection
And we did it at the household level and rural Kenya to just see how this data, whether it brings out the correct information. So that is the way we have identified and the way we have trained that data to pick up indigence and to pick up the premiums for the informal sector. Then there is the question committee setup. Yes, definitely, we will have that in the course of this quarter. We should be able to set up. One is out of our way because that is done by the Judicial Service commission. We will, of course, urge the JSC to do the setup, that is the tribunal. But the benefits and tariffs committee, we will push for its setup as quickly as possible before the end of the. Before the end of this quarter.
Tax Implications and Health Fund Management
The issue of tax. You know, there is one thing that we need to realize. We have two already funds that are tax based now that comes from the consolidated fund. We don't need to. To also put another sales tax. Sales tax generally affect the poor more than they affect the rich people. They are very regressive. What happens is when you. It doesn't apply equally. For example, if you put 1050 cent or one shilling or five shilling on a loaf of bread, for example, just as an example, and I have today, I have worked very hard and I have made 300 shillings. So if the loaf of bread was 50 shillings and you have added five shillings, you have reduced my 300 shilling by an extra five shillings. But me and you, who maybe today have made 10,000 shillings, when you reduce five shillings more from my 10,000, you don't feel it, but the guy who would have used that five shilling for something else.
The Effects of Regressive Taxation
So it affects. It's very regressive and it's not equalizes people, it just makes the poor more miserable by putting those kind of levies on certain things. That's the nature of having a specific tax on certain products. So. And that's called earmarking. We rather get from the consolidated fund for now. In the future, maybe you could go to for luxury goods and say luxury goods, we increase, or we add a certain tax and make them earmark them for health, but not on day to day things that the common man uses. I think I have touched on all the questions, if I'm not wrong. For the proximity, let's say if MBT decides to say he's an indigent, and since you say there's no enumerators, nobody to confirm whether the information you're putting is actually correct.
Verifying Data Accuracy
So how are you able now to, how are you able to now to correct, like with the actual now situation on the actual now real life situation, just to ensure that somebody is not lying on the form. So the model and the data is trained to pick the lies. So the data is trained on lies. So anytime you lie, it also is aware of that these two don't match. So your answer here and the answer here don't match. The answer here you have given and the answer you have given here don't match. So it means the data is actually trained and for us, to begin with, we rather underestimate the premium for the informal. Then overestimate it, because our worry is if we overestimate for the common, the hustler, then it will be a challenge in them paying.
Addressing Concerns on Data Reliability
But what the other thing that we are doing is if you say dispute what you have gotten, and you say, the premium is too high, then now we do the observation where now we send someone to check and confirm what you are disputing. I think this is still, like now, constructive criticism on it. There's no way you can actually verify whether the information someone has given is true or not. So we are still going to have that where you reported the chief's wife's problems. So I think it's something that you should consider. Because even like Kera, they have to go to the ground, they have to come back, they have to come to your business and confirm that this is actually the revenue you're making or whatever.
Implementing a Balanced Approach
So you can't really say that the system will detect and even AI has not gotten into that capacity. But it's okay. I think we can proceed. Of course, that's why I told you this is a start for now. And it. We rather underestimate then overestimate. That's how the model is trained for now. Okay. DJ Kroba. Yeah, Kroba. And then doctor. Then we love both Korean and Samantha to. To be our final speakers, because you're almost getting to ten. Kuroba Karibu. I see. I've seen your videos, and you're actually very passionate about this new health model. Tell us what you have for us.
Experiences of Patients Receiving Dialysis
Awesome. Thank you. Thank you, guys. Mine is. I come in for context. I come in as a caregiver. My partner is a dialysis patient, and I'm gonna narrow in on that particular sector. Just the other day, we received communication from a couple of dialysis centers where they were going to collect their mous contract from Shah, and they were being siphoned, you know, and it's a very unfortunate situation, because, unfortunately, today someone died. Because they didn't do dialysis this week. Twice. And so I would like, you know. I would like just feedback on that. Because we shouldn't be siphoning medical institutions.
Systemic Issues in Healthcare Management
That are taking care of these kind of patients. And all of us know that these patients can. All of us, even me. I can't afford dialysis for a whole month, and I. And it's bloody expensive, and so I would want feedback on that. Secondly, went through the new chief part about. And the transplant area was very vague. It wasn't very clear. I'm not sure whether you are capable or you have a team on that end that can respond. But I don't want clarity on that because now it has changed from Nhif to shif. Thank you. Yeah, chairman, you can respond directly.
Transitioning from NHIF to SHIF
Okay. So that is for me. Okay. I can ask just before Nimbo. So let me answer on the issue of. I haven't understood the part of siphoning, because unless you mean facility has lost money or something, but what I know is in terms of the rate, we have increased from 9600 to 10,650 to the facility. So the siphoning part I haven't understood. But the issue of what I meant. By that was some facilities are being told to pay up to get their contracts. I'm sorry, I might have said the word symphony, but that's what I meant. No, that is unacceptable and that's wrong.
Implementing Changes for Improved Healthcare
Because what we. And that's the reason why I was saying that we have changed the model of contracting. Empaneling is within 30 days if it's a new center. And contracting is supposed to be online. So you don't need to pay anyone. There's no discussion. You don't need even to know who is your branch manager. You fill in online and you send the contract. And that was the idea of the e contracting. And that's what we are going to do for physical contracts. It's a temporary measure, but the e contracting is what we are supposed to do on the issue.
Enhancing Access to Healthcare Funds
No one should pay. And I think that we have made it clear that no facility should pay anything for being contracted. And that was the whole idea of publicizing these things on the website and saying, this is how you proceed on the issue of transplant. So what we have done is, for the first time, there are certain things that we said we are going to pay for. One of them is pre transplant evaluation. This was not there previously. And that means that we pay for the pests that are required, for example, the HLA typing and what people are paying out of pocket in NHIF.
Supporting Transplantation Procedures
But for now, we are saying the evaluation and the testing, because they are damn expensive, is around 150,000. So we will pay for that matching. Two, we are paying 700,000 for the recipient, the surgery. Three, we are paying 168,000 for the donor. So you see, previously were paying around 500,000 for the recipient only. We are not paying for the donor, and we are not paying for the pre transplant evaluation. Now we are paying for the transplant evaluation. We are paying 700,000 for the transplant.
The Financial Impact of Healthcare Changes
For the transplant patient, we are paying 168,000. So if you look at these figures, that alone is 768,000 plus 150. It's almost a million. Previously, the amount was 500,000. So a million. Now, public facilities should comfortably be able to do this transplant without any challenge, because they used to do it at 600, 700, 800,000. Now, even for private facilities, a million is reasonable enough. And we might get one or two big facilities that are willing to fit in within this price and provide transplant to patients.
Post-Transplant Care and Treatment
But what else have we introduced in this space? Previously, you could undergo your transplant, and then after that, you are let go. What you needed is medication, post renal replacement therapy. And that was also very expensive for the patient. Those drugs are unreasonable in terms of their prices. But in this new package, we said we will pay 200,000 for your post renal transplant medication, which was not there. So as a package, if you look at this space, Shah will pay almost 1.2 million from the donor to the pre transplant evaluation.
Understanding New Healthcare Packages
Transplant plus post transplant medication, we will cover. And that's what is in the tariff. I hope that is now clear. And this document, I just want to tell people, is a public document. If you go to the Kenya Gazette, you will just find it and download it. And it clearly spells out even the rules, the what, where to get this, which kind of facilities, the amount. So that when you go to a facility and they tell you Shah is paying for you 600,000, you should be able to say, no, the document says it's 700,000.
Fostering Transparency in Healthcare Funding
And you report them to Shah and say, there's a facility here that's saying it's 600. But what you have published on your tariff is 700,000. So that's the kind of transparency that we are advocating for sure, where the documents are easily available and everyone can see, and they are in public domain. Nothing is under the table. Thank you. Thank you, chair. I want to bring Doctor Karama and then Eboso. Then. You love Korean. I have two speakers we close for. Thank you very much.
Experiences from the Field
So, number one, I have a few comments. I'll try and be as fast as possible. Comment number one. Doctor Mbiti, thank you very much for the work you're doing. I am very proud of you. I've been observing you even when you're going through the fire, you have been rock solid. Asante sana, continue. I think you are the future number two to the chairman, our chairman, Abdi. I thank you for the good work. And I wish you the best. I think we're on the right track, to my point. Number three, when were younger, when were trying, when were singing yote, I was a kana bila nyong'o.
Addressing Historical Challenges in Healthcare
One of the biggest challenges that we had then was we needed everything to work for the doctor. And actually, on this point, I'm going to be addressing doctor everyone, but particularly my good friend Doctor Chibanzi. When were younger, we used to agitate and say, we need two things. In fact, my colleague, Doctor Vikrangani used to say two things. We need to make sure doctors are paid. And number two, we need to improve healthcare. But what am I seeing now? I mean, at that time, we made so much noise and our objective was to bring the conversation of healthcare to be front and center.
Advancements in Healthcare Conversations
And most of us here who were in the streets and singing those days, and all we wanted was to make sure that the conversation of healthcare was front and center. And President Uhuru immediately thought about UHC and most of the conversations that started in 2014. And eventually, when our colleagues, Doctor Ouma Oluga took over, the conversations became stronger. And louder in healthcare. And now we have a head of states who has made healthcare their number one agenda. For me, that is extraordinarily gratifying. But I'm quite concerned that the direction we are taking, we have become very, I don't know which word, very unfriendly to the entire topic about healthcare.
Concerns About the Direction of Healthcare
To a point that if I. Is onyimbo still around. Yeah, I'm a potaya. Please tell me you can hear me. Yes, we can hear you now. And the way I was talking for a long time. Let me start again. So where did you hear? What was the last thing you had? Oh my goodness. So I was saying, I have faulted our bosses, Doctor Davji and Tim, not because I think it is the noise that we made in 20 12, 20 14, 20 17 that made it possible that healthcare is now a conversation front and center.
Trust and Transition in Healthcare
And you can see the union is. Now actually working for healthcare. You can see Abdi is there as our boss in Shah. We can see doctor Thoranila in Statehouse. I think we have succeeded in what we wanted. We said that being in the streets is good, but being in the decision table is perfect. Now we are in the decision tables. But I think even when we are making decisions, most of us don't trust the decisions that we are making. So I want to go to the topic the second, the third topic, or is it the fourth? The fourth topic is about NHI.
Reflection on the NHIF Transition
Yeah. So, one of the reasons why I am happy about the NHIF being cancelled is NHIF had lost its character. We know that there is a social health insurance where the many, the rich will contribute, so that the poor can also get. That's a social health. And so, generally, universal healthcare should be funded either through contributions or taxes. And therefore, the people who have more will give, so that those who have less can get.
Distinguishing Healthcare Model Approaches
And so the character of a social healthcare is not that you get a commercial product. Now, NHIF, from somewhere in 2013 or 2014, they started giving commercial covers. So you have a social health cover, which is giving commercial products, and we call them enhanced covers. I think the reason why we even calling it a social health care is to remind us that this is a social health cover and not a commercial cover, like the jubilees of this world and. And the madisons of this world.
Discussion on Fund Distribution and Coverage
And so I think this is a great distinction. And I think Doctor Ouma was asking why. And the man from. From Pocot was asking that, why is he not getting the comprehensive cover he used to get? What the man from Pokot was getting is something called a commercial cover. You give money and you get value for money immediately. What Shah has to do is get. 100 shillings from 100 people, and then.
Explaining the Social Nature of Healthcare
Cover that with COVID 300 people, using those 100. So 100 people contribute, so that we can cover 300 people. And so it is not a commercial. Product, it's a social program. And that is a very great distinction under which Tibanzi would. Because the other speakers had some questions, and I think Doctor Abdi had gone into depth about that. Let me finish. Let me finish there. I can just finish by saying this, Doctor Abdi, my anxiety is, why did we choose to use contributions instead of taxes?
Critical View on Contribution-Driven Models
I feel like a contribution funded UHC can be a challenge. I think that is the short question. Thank you. So, just to answer that short question, thank you for your contribution. We have done a mixed model. And let no one lie to you that one model of financing is better than the other. Social health insurance is usually the best method of providing UHC. But for us, what we have done is we.
Financial Structure for Sustainable Healthcare
We used both tax and contribution tax to cushion the contributions, because we know contributions alone will not be able to give us all the benefits and the tariffs that we need. And it will not also add the rights, some of the rights, like emergency. So, for that reason, we have a mixed model. And I think that is what will make us sustainable. Because you also don't want to burden one part, which is either a contributor or which is just tax funded.
Discussion on Taxation and Healthcare Funding
And let's keep in mind that our health system currently, as it is tax funded because people, you know, sometimes confuse these things. As we speak today, the Ministry of Health gets a budget. Counties get money. Actually, most counties, because health is devolved use, the highest percentage of their budget goes to health. But you tell me whether that is giving you any value. Number one, two, whether it that is sustainable.
Output-Based Financing Mechanism
How much more do we need to pour into that line of thinking for us to get value out of it? So this model also, the other thing that this model has done is, other than being tax funded and contribution is we have made the financing to be, the financing is output based financing mechanism. So it's not input, it's not brick and mortar, it's not equipment, it's not. So what we want you is you provide the service, I pay for the service.
Ensuring Quality of Healthcare Services
And at least I am sure the patient has gotten the service. So I'm paying for what the patient has gotten, which is a service, a healthcare service that they needed. But if we move towards the input financing which we have and have been having for the last 60 years, we know the outcomes and we know the results. Thank you. Thanks, doc. We have been 2 hours to entertain, so I have four speakers.
Transitioning to Efficient Healthcare Systems
I want to bring Aboso. I know he has a lot to say. He is quite insightful on these issues. Then I'll bring Coram, then the two doctors. Okay, thank you very much. Number one, I'd like to tell doctor Abdi, who's my friend, and we've had several discussions on this shift right from last year, that I'm still not persuaded on why NHIF could not be made better, but. Well, it is what it is now on.
Concern Over Transition from NHIF
The first issue is on the issue of transition between chief and NHIF. When were giving public participation views in February or March 1, of the issues I raised in my memorandum to the ministry was a transition. And I pointed out that health is a very important function and that we have to be careful that we do not allow the NHIF to be wound down before we have really transitioned properly. I think I even proposed that we could start launching the social health program by region, so that it can be tested in one region, then another, and then another and whatnot.
Smooth Transition Strategies
So that there is no interruption. I don't know if that was ever really considered and what came out of it. And even right now that anyway, the NHIF act will stand repealed next month on 23rd. But the services and what NHIF has been doing really is being taken up by Shah at this point in time because of the hiccups we are getting. Is it possible that the shire board can still continue providing the NHIF services even as Shah, exactly as they were, and roll out this shift now regionally so that we don't have a situation where we are having these hiccups?
Analyzing Cost and Contribution Dynamics
Number two, the issue of cost versus contribution. Now, generally in public health, I think when we study public health, and I think even in law, health is not considered a public good, strictly speaking, health is generally considered one of the things that you should pay for privately. But government can be involved in providing health and providing health policy and regulating. But here we have a situation where we are essentially making health a public good.
Shifting Definitions of Public Healthcare
There are good things about it and whatnot. But the problem with that is we are making not just the healthy to ensure the sick, we are actually making the wealthy to pay for the poor. And it is not government doing it. It is actually an individual who's taking care of the health of the community. And really that in itself, I think is quite offensive to. I know it's been said as though it's a good thing. It's being said as though it's something to celebrate that we are taking from the rich to give to the poor.
Concerns Regarding Equity in Healthcare
That's not okay at all. And I would like to just point it out at this very stage that it's not okay to take from the rich people or those you consider wealthy in some way to give to the poor. It is government supposed to provide these services through taxation or through taking care of the indigents as it is and whatnot. Kenya is not the first country to have social health insurance, because I know India, Singapore, China have a form or another of the same.
Examining Successful Models of Healthcare
I think the nordic countries provide for this through taxation. But Singapore, India and China all have a social way of sorting it. But even then they have categorized the health, the different packages, such as the benefit, so that there are those, the poorest who have their own fund, that the government invests more in it. Then there is a middle income and then there is a very high income. And it's because it's just, we are talking about equity and being fair, but it's not fair for one person to be paying 240,000 per year or one household, and then they get the same as someone who's paying 300 bulb per month.
Challenging the Healthcare Contribution System
It's not fair. And that same that they are getting is really not really adequate healthcare, if I should say so, because there's a maximum that you can get from it. As you pointed out, someone on dialysis will only get a maximum of 1.2 million. So someone who probably would want more, maybe would want even to go out of the country, or would want to get private healthcare even, and can afford it. Why are they still having to pay all that money to share and whatnot?
Examining Disparities in Contributions
Then the issue of the means testing and the differential ways in which salaried people versus non salaried people. People are being made to contribute. Salaried people. It's being taken from their income. Non salaried people. And I think there was some misrepresentation that the means testing is for indigence. No, it is actually for anybody who is not on a formal salary. Now, I know very many people who are not on the formal salary. I don't know.
Inequities in Means Testing
Someone is. I know many people who are not in the formal system, but they make a lot more than the formal people. A businessman, for example, who is not employed, that person could be making a million a year. But then you will use a means testing tool for them, and through the means testing tool, they may pay much less and whatnot. And aside from that, when you take from the salary versus from means testing, what you're doing is you're taking my gross before I have paid school fees for my children, before I have paid my rent, before I have paid anything, you're taking that money from me.
Concerns Over Data Collection Methodology
When you use the means testing tool to determine the items we have in the house, like a tv, two toilets and whatnot, those are items that we purchase after we have taken care of other basic needs that's not being considered. How did we arrive at 2.75%? Why not 3%? Why not 4% or 20%? Why not 1%? That 2.75% was determined. I know before even this government got into office, when it was still campaigning, they talked about 2.75%.
Evaluating the Decision Behind Contribution Rate
So when 2.75% is implemented now, it seems to me that there was no mathematics that was done post getting into government and seeing the realities that this was just transferred from the manifesto into the regulations. And really, that's not how we should be dealing with public affairs, because these are people's individual monies and these are people who are already struggling on the question of data transfer. Again, I wasn't really persuaded, and I was a bit.
Concerns Over Privacy and Data Security
I frowned upon the fact that the position seems to be that if someone feels like their data has been infringed into, they should go to the data protection office or go to court. I don't think that really should be the attitude, because essentially data and privacy is very important, especially because we are going to run this data over a system that is one not being managed or not being owned locally, or that has not been developed locally, that will have access to third parties, that we don't really know what other things will be done with this data.
Need for Transparency in Data Management
And so it shouldn't be a casual approach where a gazette notice is just put out, in fact, without public participation. And by the way, I don't think the parent act that authorizes the gazette notice contemplated a situation where NHIF data would be automatically transferred to Shah, because there's nowhere along where the issue of data is talked about. So I think it's something that Shah needs to relook at. And if the attitude that Shah is going to have on personal data is to that the way it is coming out, then we are even more worried that we may not really trust now, Xiao, even with the data, including even the one that we give consensually.
Addressing Healthcare System Trust Issues
Then Doctor Abdi talked about the issue of regressive NHIF and progressive in terms of the contributions and whatnot. And I'm starting to feel like Shah is delving into very deep and controversial political and economic issues that even the world generally struggles with. Shah is talking about. I mean, he said, this whole idea that is coming out is that part of what is underlying Shah, we should just be an entity dealing with health. It's talking about communist aspects where rich people are taking care of poor people, or socialist aspects.
Navigating Political Financing Challenges
They're talking about sort of like determining the taxation regime and sort of trying to determine whether a tax is fair or not fair and whatnot. And I'm starting to feel like health is too risky. Health as a public thing is too risky to start subjecting it to this kind of experimentation where we are trying a new way of taxing and whatnot, or we are trying a new way of managing consumerism. Because I think I heard you talk about how we are going to talk about the commodity prices and whatnot, and how to bring them down.
Concerns About the Future of Healthcare Funding
I don't really think health, especially health that covers the whole country, is the place for us to try those things, especially not at a go. So I think those are the concerns that I have that Shah should try and steer clear from trying to determine taxation issues or how many people in the formal sector contribute to tax and not because we will go wrong. Tax is so broad and so such a serious political question and a very, a global issue around the entire economy that we might collapse healthcare because of trying to experiment in such things.
Concluding Remarks on Healthcare System Transition
Thank you very much. Thanks, Malimu. I think, chairman, you will respond. I wanted to bring korean doctor Mohammed, then I'll bring Chibanzi and. And our KMA chairman. As the health speakers coriander, we share. Actually, the statements that he has is exactly what I were my concerns. It's okay. I know Boso is my friend and he's on a speed dial, so he can call me anytime, any minute. But more importantly, I was hoping also when we raise such issues, I think.
Addressing Immediate Concerns in Healthcare Delivery
You know, I have noted. You see, those are. What did you call it? Philosophical political taxation. You see, the. For me now, I was trying just to answer the issues that the day to day things, in terms of how. How do we address the operations, in terms of how do we make sure the transition is much more smoother. And we conclude as fast as possible, in terms of the transition. And then how do we address the. The hiccups.
Education Funding
But those get their fair share of and even more education receives up to 700 billion annually from the exchequer.
Health Budget and Administrative Costs
Health is the first time that we are saying we need something extra other than what was previously budgeted for. So the second thing is because we are collecting now premiums from both formal and informal, so there will be enough resources, there will be sizable resources at share, but more importantly, the administrative cost is capped at 5%. And secondly, we don't have the leisure of investing. So the work is just to pay providers. So we can't do land and such things that NHIF used to do.
Role of Private Hospitals
So we are aware and we are alive to the fact that private admission hospitals play a very crucial role in health service delivery. If we looked at our press release on Sunday, it was after we had a discussion with those providers and I can tell you, majority of them have already signed the contract. So we don't have any preferences on who provides the services. As I have said earlier, it's output based financing mechanism. So it is who provides services is who is paid, not a budgetary allocation to specific facilities depending on the ownership.
Payment for Healthcare Services
So for us is money follows services that the patient has gotten. So you are saying county that has two public sub counties that has two public facilities. I can tell you Nairobi, I think it's only 15 or 17% of the facilities are owned publicly. 85 or 83% is in private admission hospital hands. So we are alive to those facts and we know there's no way you can run health without the private and mission facilities. There are plans. There was a payment that was being made today. If I'm not wrong, then there will be subsequent payments which was the pending bills for NHIF, which will be done next week and hopefully another one the other week.
Funding Uncertainties
So we will have maybe the next three to four weeks. We will have two to three tranches of payment for pending bills from NHIF. I think I have tried as much as possible. Yes, yes. The last question was in about two weeks or three weeks time. The court we have are already. Oh, okay. The. Now. Okay, okay. Yes. Now we have service providers who will be operating with a contract. They have just signed a contract recently with Shah, but now their previous contract with the NHIF because of the act, it's already null and void.
Legal Questions and Service Contracts
Now we are working in a void that we don't know. Do you provide a service without a contract or. So what plans are there? So the plans is every facility has been given the leeway to sign the contract or exit. So what you need to keep in mind is not every facility is run by the owner. So some facilities, it is the administrators who are in charge who have to get approval from the owners whether to sign or not to sign. But on the issue of the court, I think we allow the court to make that determination.
Judicial Oversight
But if you have read the ruling of the high court, you will see the high court was very categorical in terms of what the issues were. So they talked about, I think, three issues. One was the issue of emergency. And for me that was just an error because they said and thought that we have denied, we will deny people emergency services because they are not registered. It's very clear in the regulations and the laws that emergency is for everyone, irrespective of their registration status and their.
Public Participation and Future Lawsuits
So I think there was an oversight in that from the ruling. The second thing that they talked about was the issue of public participation and sensitization. And they said it was not adequate. They did not say we do not do public participation, but they said it was not adequate, that we should engage more and sensitize the public. Then the other thing that you need to keep in mind is there will be many more lawsuits. So if you say we will not proceed or will not do anything, then you will get stuck because everything will be canvassed in the courts.
Court Determinations
So it's the courts who will make that determination, not for us to say we can't proceed because there is a court issue. So the court will look at what is in the public interest, where are the issues that need to be addressed and what is coming out in terms of the interests of the public in general, and you have a chance to be heard throughout. So you have started from the high court. You are in the court of Appeal. You can move to the Supreme Court.
Expectations from Healthcare Reforms
So you have that right of appeal process to go through the court for it to make that final determination at the apex court. So for me, I would say that let that take its own trajectory and we'll find out how that ends up. Thank you very much. Thanks, doc. I think we are way past our time. Want to finish? Let us go top of the hour. I think we'll have subsequent spaces. I also work in a mission hospital.
Personal Experiences in Healthcare
What Korean is saying is what we're experiencing right now, like I said, we only have four patients. There are a lot of logistical issues. The hospitals themselves are very, are not very willing to admit patients for the fear of losing out, like our facility. NHF owes us quite some huge amount of money, not even to talk about Linda Mama. So I hope we love these subsequent conversations, purely non political, very objective on it. I want to bring my doctor Chibanzi, and then I have my KMA chairmani.
Healthcare System's Financial Viability
And then we love the two doctor strange and Mohammed, as we wind up Chibanzi Karibu. Thank you. Well, I think I just say that I've listened to my good friend Abdi, and we've had conversations before, and I agreed that we are diverging on how this entire thing is being financed and being run. But nevertheless, I'd keep it very simple. I don't want to discuss so much. I think the question I have is, first, is clarify the NHIF comprehensive cover came into being when civil servants relinquished their 3000 medical allowance.
Understanding NHIF Payments
There used to be a medical allowance before, so there was a 3000 medical allowance plus the 1700 that was being deducted from the salaries. So it was not 1700. The total contribution from civil servants per each civil servant was 4700. And that would perhaps explain why they were getting much more benefits as opposed to other Kenyans. The issue of inequality and equality is a whole different discussion and debate. But having clarified that, I had Abdi say that the deficit was 3 billion, because he said expenses were 9 billion, contributions was 6 billion.
Addressing the Deficit
So the question I have is this, how much would it have cost despite the 3 billion it will have meant then, if you want to cover this deficit and the civil servants, according to your reasoning, were paying less than it was coming from the other port of other Kenyans, if you were to increase, for the civil servants to cover this deficit, how much would you have increased? One and then two. If you would have decided that you are rolling out this comprehensive cover to the entire population, how much will it have cost? Those are my two questions.
Financial Projections and Coverage
Simple updates. Is there, I think you can respond, because there are quite precise questions. Okay. So you, of course, if you needed to cover comprehensively the civil servants, all the other schemes that were loss making, by the way, it was not just civil servant. There were 96 schemes. So it's not just civil servant. But more importantly, unless Chibanzi knows something that I don't know, not all civil servants earn more than 100,000. So 1700 was for doctors and other caddas, other higher job groups.
Collective Financial Responsibilities
You know, there are those lower job groups, KLM and what. So their contribution was not 1700, it was the usual 800, 400, 600, 1200. So you needed an extra 3 billion for you to be able to cover comprehensively. So if one around and the civil servants were 135 members, thousand with their dependence. The rough estimate was around 400, or make it even 500,000 and then make 10 billion as their requirement. So I will do for you the find x.
Estimating Future Healthcare Needs
If 500,000 consume 10 billion, how much will 50 million consume? That will give you the figure that you need to give that kind of comprehensive cover to the whole Kenyans. But generally speaking, and the reason why that was if you take that route is remember civil servants who are getting benefits and they are accessing it through the private sector. If you limited them to public sector, you wouldn't need more than the 6 billion that they were consuming, that they were paying.
Healthcare Service Costs
You will need actually much less. Why do I say so? The reason why I say so is if you go to the private sector, for example, to any major hospital, and you go for normal delivery, and you take your wife and you say, I want her to deliver, you can pay four prices for the same process of normal delivery. Four prices. I did not say cost. Please underline the word prices, not cost, because it depends on where your wife will sleep.
Market Influences on Healthcare Pricing
It is the hospitality aspect that will determine how much you will pay. If you go to the general one, the delivery will be maybe 50,000. If you go to semi private room where you are sharing the washrooms, you will pay 100,000. If you go to private room, you will pay 150,000. If you go to the presidential suite or whatever luxury rooms they have, you will pay 200,000. You realize that this same woman would have been delivered by the same nurses in the same labor ward using the same drugs, but the only difference is where they have slept.
Healthcare Quality and Accessibility
So the civil servant scheme was expensive or they were consuming more than they were paying is because of that kind of access where someone says, I have a limit of a million, so let me go to the presidential suit for my treatment, rather than a general ward or rather than going to a public facility. That's what made it expensive and unsustainable in terms of what NHIF was paying. So we will not go that route of find x.
Sustainability in Healthcare Funding
If 500,000 is using 10 billion, then 50 million will use times whatever. It will be irresponsible of us. And that's why we have these benefits and tariffs, and that's why we are saying this should be available in both public private sector. So if now you need now those kind of hospitality aspects of those services, then you should be able top up either from your pocket or from your private insurance.
Public and Private Healthcare Dynamics
But for us, to begin with, we want to do to provide the basics and certain aspects of this package don't need the hospitality. As like, if it's dialysis. And that is fixed for everyone. And they are able to find it from anywhere. Public, private mission for the same price. Cancer, similar radiotherapy, PET scan, similar prices without having top up. So I am not saying they did not concede their allowance.
Addressing Healthcare Inequities
What I'm saying is their allowance plus their contribution was not enough for what they were asking. It was not sustainable. Thank you. Thanks. I wanted just to bring Keme Taiman, Doctor King Mohammed and then. Strange when we love Karen. Yeah. Thank you very much for the organizers of this space. And I think one of the most important principles is that we must continue discussing.
Healthcare Discussions and Participation
As you know, the KMA board person was not put into the board until recently. So for us, as KMA, we can. Say we have not contributed to say until I became chair. Yeah. So we know that the KMA person has not been. And therefore the KMA input has not been considered. And that's why we are having some of these problems that we are having.
Politics and Healthcare Transitions
So let me tell Abdi that no one should die for a transition. So that people can say they have transitioned from Shah to NHIF in one day. And I think from the realities on the ground, we should not run away from the fact that this transition, the change management, was poor. So let's see how to solve that, then. Secondly, of course, the Robin Hood principle.
Healthcare Funding Models
The OECD countries have agreed on tax principles which constitute of equity, efficiency, simplicity and transparency. The Shah system goes against all those. In terms of equity. They. They keep yapping that 2.75% is equitable. It is not in the principles of equity. In tax principles, you have an inverted triangle, such that the people who earn more, they get taxed at a lesser percentage.
Taxation and Income Disparities
Of course, the total amounts will be less. Of course, we have proposed that they cap it at a certain figure. But at the end of the day, we think that we should not even be paying on a gross salary. And why should we not be paying on a gross salary? The government, the Kenya Kwanzaa government is in charge of the country. It has caused the cost of living to go high.
Economic Challenges in Health Financing
So the gross income of any person does not reflect their means. Over the last two years in the Kenya Kwanzaa government, the bank interest rates have doubled. What does that mean? Some of us who had credit facilities and mortgage facilities are paying double what they used to pay in the previously stable credit facility and mortgage interest.
Impact of Economic Policies on Healthcare
So what does that mean? It means that this gross thing that they are talking about is nothing so secondly, the government is also in charge of things like education. They are the ones. If you have poor quality public education, people have to move to private education. Nothing of their own making, but as a result of the government, so for the government to come again and to charge extra, so you become the government supporting so called other people because you are perceived to be rich.
Concerns About Fairness in Taxation
That's, I think, triple taxation. It's not even double taxation. Thirdly, they say that you pay as individuals, but benefit as a household. I think that is Robin Hood. That's Robin Hood. You've taxed the father, the mother and the 25 year old child, but when you come to claim for benefits, you are being told 900 shillings for the household, but they have charged you for three people.
Transition Challenges in Healthcare
So I think that is not fair at all. And for this transition now, the current one that is having the facilities, it's obvious that the system is not working. And for people who are seeing patients, and they have experienced this in 2019, when NHIF switched off the systems, is that you will not be paid for things that have not been captured by the system. So a system failure makes you a contributor.
Impact of Systems on Service Delivery
You become like CSR of government. And that's why a lot of people, and you have had some of the faith based organizations saying that they will not see people until they pay. It's because of previous experience. So I think they should move fast to solve this transition thing, which we, as providers had said that they should take over a year or two to try, but I think they just want to change quickly, just to say they have changed quickly.
Future Discussions on Healthcare
So I go back to my finally, OCD tax principles. Equity, you should have an inverted triangle. The people who earn hire should pay a lesser percent, or at least according to our propositions. We say you either cap it or remove it so that it be fully funded. Efficiency. We need to minimize economic distortion of these taxes. Simplicity.
Transparency and Fairness in Taxation
The means testing instrument is not simple and it is not verifiable. So this goes against the trans. Finally, transparency. The means testing instrument is not transparent because I can come, community health worker comes, I tell them right there that I have attached house and you get less payment, of course, because of the economic conditions that are as a result of the government.
Recommendations for Tax Cap
So my advice to Abdi, either cap the deductions or remove them because this is extra taxation that we cannot handle then. Secondly, we need a transition period so that people do not. This thing will be thrown out based on access to patient care because people cannot access, because a system is not working.
Healthcare Accessibility and Digitization
But overall, finally, just to say that I have looked at the overall system of the digital superhighway and I think. It is a brilliant idea. But some of the issues that are not being addressed in a small component of this whole thing called SHa are the ones which are messing up a brilliant idea.
Healthcare System Sustainability
So I think they need to be looked at and we'll be passing our message through our representative at the shabboard. Thank you very much. Thanks. Before Abdi, you respond, I think Kush also had. He was here before and they dropped. He had an idea on something close to what KEMA president has, maybe because you can have two minutes or three, and then we bring Doctor Strange and Mohammed to close for us before we give the chairman.
Expression of Gratitude
Hey. Hi everyone. I hope I'm clear and audible. First of all to Miti and especially to Doctor Abdi. Thank you for giving us this time to be able to discuss such a critical topic. So I'll start by making a general comment. Doctor Abdi Ameseman Ogapa philosophy. So sit up on that.
Clarifying Healthcare Funding Structures
But I think I feel like in this whole discussion, there is something that has never been clarified in our society on how to deal with healthcare delivery, healthcare financing, etc. Just to address the point that doctor Iboso made. Most societies consider healthcare to be a private good that you pay for your own healthcare.
Government's Role in Health Systems
The government is there to regulate and cushion the less fortunate in the society. We have never really clarified where our position is as a kenyan society is on this. We have a mishmash of both. We have a government program that is supposed to be competing with private healthcare facilities, private insurance, etc.
Comparison of Healthcare Systems
If you are to look at the split between public and private facilities in Kenya, it's around 43% public facilities, 37% private facilities. Comparing this to like more advanced healthcare systems, for example, the ones that are doing universal healthcare, especially if you look at the UK, for example, with the National Health Service that they have.
National Health Services Comparison
The National Health Service operates 87% of public facilities, 13% is left to the private facilities. And none of those facilities are involved in critical care, in emergency care, in basic care, in primary care, all those components are fully taken up by the government. If you go to Netherlands is a similar thing.
Regulatory Frameworks in Healthcare
You have private entities, facilities themselves, insurances that are operating under a strict regulation of the government. The government actually makes sure every. Every resident in the Netherlands pays healthcare premiums. If you don't pay healthcare premiums, you actually find. But then again, if once you pay the healthcare premium, you are guaranteed all levels of basic care.
Understanding Healthcare Premiums
If you get into a car accident, you get all the care that you need. And you go home. If you are to deliver, if it's a pregnant woman delivering a child, they deliver the child and they go home. Comparing this to the opposite, which is the best example, is the United States, where we don't have. There is no major role for the federal government or the state government, individual state governments, in actually providing public health care.
Public and Private Healthcare Balancing
The government is strictly involved in regulation and protection of the less fortunate, the elderly, the homeless. So in Kenya, we are kind of in two minds about it. And this is coming out in all these discussions we're having about the shif and the primary healthcare fund, where you have a mandatory fee.
Challenges of Mandatory Healthcare Fees
Some. At some point it comes out as it's mandatory, but then you have to register. But then there's also an element of it that is covered by taxes, but then the COVID that you're getting that is mandatory is nothing, is nowhere near enough to cover basic healthcare.
Insufficient Coverage for Healthcare Needs
Telling a woman that you're going to cover her 10,000 shillings to deliver a child, that 10,000 shillings will be over by the. By the time the woman gets to the delivery room, will not even cover the charges for the delivery itself until air postnatal kitc. So I think there we have a big problem as a country, and not necessarily, this is not necessary to Abdi, as the chairman of share, but I think because he has this privileged position as the custodian of healthcare financing in Kenya, he needs to really take this into account and consider it.
Strategies for Reducing Out-of-Pocket Expenses
That leads to the strategies that we should be taking to reduce out of pocket and cash pay. Because as you all know, probably 70, 80% of Kenyans are one medical emergency away from poverty. I work in a critical care environment where I see this every single day. Someone comes in with a stroke, their whole family is bankrupted within a matter of two weeks because they cannot afford ICU charges, they cannot afford the critical surgery that the patient needs, etc.
Social Health Act's Role
So, as we know, discussing all this, it needs to come out clearly that the role of this social health act is to reduce the amount of cash paying that we're doing. I was taking a look at the document called tariffs to the benefit package under the Social Health Insurance act that's in the Ministry of Health documentation.
Review of Healthcare Packages
I'm not sure if that's the correct document to be looking at, but that's what I found. And as I'm just scrolling, I'm. I'm seeing many places where you have limits of four visits for outpatients, limits of 900 person, limits of two ct scans. You see? So you're taking, you are essentially tax the population and putting them in a situation where they are paying a significant amount of their income.
Comparison with Private Insurance Options
If you are to compare it to, for example, private insurance options and giving them probably like 30% to 50% of what is available in the market, this is not acceptable. It can't be acceptable. Again, another point that Doctor Iboso raised as well as chairman raised this strategy, this Robin Hood strategy of equalizing through inequality, because there are people who are rich in the society and others are not as rich in the society.
Potential Class Divisions in Healthcare
We have to make the rich pay for the poor. Not only is that not beneficial to the society as a whole, because the rich will start finding ways of. Of avoiding paying that, paying their shares as they're required. You're also introducing. You're introducing this idea that there is a class that should be paying for another class and you're introducing a whole new class, or that I don't think is beneficial when you're discussing healthcare matters, I'll just raise one or two issues that I've seen in the three funds, the shif, the public health care fund, and the Emergency and critical illness fund.
Implementation Challenges
Most of the things have been touched on by the previous speakers. There is the issue of the poor implementation. It was too rushed. I wonder what was the rush to roll this out essentially overnight, when you could have had a staged rollout to make sure all these teething problems are being sorted out as we go. That was really poor. We have these.
Legal and Constitutional Battles
All these legal and constitutional battles that are going on. I won't comment much on that. There is the issue of the mandatory nature. You're making people pay essentially by force. You're targeting the salaried individuals because you can get to their money. You're creating means testing tools to find ways to make mama boga and boda pay their share.
Addressing Coverage for All Individuals
But not only are we not having enough coverage for the different medical emergencies and medical illnesses that you have, we also having a clash. For example, if you are to look at that document in the maternity and newborn and child health services, the same charges that are supposed to being covered by the public health care fund and the tariffs that are being offered are the same ones that are being offered in under the Social Health insurance fund that now is supposed to be replacing an HIF.
Overlapping Coverage Issues
So if I'm paying taxes legitimately entitled to the public health care fund, why then am I being forced to pay for shif and getting the exact same service at the exact same price? It does not make sense to me that overlapping coverages. I don't know what. I don't know what was the idea there? Or maybe you can clarify, chairman, the last thing, and then probably the most important point I'm going to make.
Corruption Within NHIF
The problem with NHIF was not the structure. Maybe there were issues that needed to be streamlined, maybe there are issues that needed to be upgraded or reformed. But the primary problem was not the structure. The primary problem is corruption. Just like any other public health, public institution. We have people who are working there, who are buying apartments in Lavington, who are taking money here and there, taking money in SAC CTC, so we can paint the boat.
Addressing Systemic Issues
But if the boat has a hole in not going anywhere. So I legitimately see us in a situation where by the time it's getting to 2025, 2026. I'm sorry to use your name, but I would hate to see you in a situation where you're being summoned by ACC because 5 billion shillings has grown some legs and disappeared.
Combating Corruption in Healthcare
So how are we going to deal with these issues of corruption? We might talk about this digitization issue and everything. Already the digitization has a question mark about the tendering that was done. If you were to look at the other places that have been digitized in the government, we digitized pay slip systems, but we still have ghost workers, we still have double payments, we still have all these problems.
Addressing Systemic Corruption
So cosmetic solutions to a systemic problem will not get us anywhere. That's all I have to say. Thanks, Kush. I think that was chair you have to respond to Kush and the chemist. I think they synchronized the opinion, which most of us actually share, and they're actually very, very important.
Final Remarks and Summation
So you'd give us your. I want us just to sum up, because I don't want, again to bring. I want Mohammed to say something. Hope chairman is noting them out as he responds to them and his closing remark. I think that will save us time. Moha.
The Importance of Dialogue
Hello, everyone. I hope you guys are okay. Thank you, doctor ambitides, for this platform. Thank you, doctor Abdi, for being. This is one of the rare occasions where we get someone who is on the decision making table, allowing us to have room for discussion. And I think this is something new. That Doctor Abdi has brought.
Clarifying Healthcare Delivery and Financing
So my questions are not many. Just three questions. One to Doctor Abdi is how long. Are you anticipating these teething problems to last? And if you can give us like an estimated timeframe of when the system will be working flawlessly. The second one is in terms of.
Financial Projections and Future Planning
Financial projections, in terms of projections, in. Terms of finance and number of registered people. What are your projections for this quarter? And are the projections enough to cover the NHIF debt payment as well as payment for services under share without accumulating any debt to Shah or overburdening the facilities that were already having HIf debt with now new debt to Shah?
Personal Insights from Leadership
And finally, this is to. This is more of a personal question to Doctor Abdi. What is the one thing you like most about Shif or Disha? And what is one thing you would have changed individually? Thank you. Thanks.
Closing Remarks
I think you can. You can respond and then give us. It's quite late. We've been here for more than 3 hours. Perhaps we should have started earlier or also have follow up sessions. You know, every time I go for this kind of discussions, it takes longer than expected because with time people learn the questions reduce in terms of what needs to be clarified.
Transition and Payment Updates
So just to answer the last, we, as I have said, that there are payments, any type of debt payments is being made which was supposed to start today. I think some facilities will receive their payments early next week. There will be subsequently regular payments to clear for the next three to four weeks.
Delivery on Financial Commitments
Not to clear fully, but to make substantial payments to the facilities for the pending NHIF debt. Then there is the issue. Yes, for sure. So there is the two funds, primary and emergency and chronic illness. So those ones are tax funded.
Funding for Healthcare Initiatives
So we have already 6 billion given in the account and then we expect subsequent allocations in the supplementary budget. But in terms of collection, our expectation is because we are looking at nine months. So our conservative estimates is around 70 billion for the nine months.
Financial Outlook for Healthcare
So if you divide that into quotas, you will find is around 16 to 17 billion quarterly. Then in terms of what do you like about the current shah? Two things. One, we are operationalizing emergency as a right, 14 years late, but we start from somewhere.
Progress in Emergency Healthcare
For me that is something that I'm really happy about it, that for the first time at least, you are not worried about emergency treatment when you are involved in an emergency situation because you don't have money or anything. Second thing for me is the primary health care.
Primary Healthcare Outlook
So the primary health care also is something that I would say will touch many people. If you address primary healthcare properly in terms of service, availability and provision, which I'm not saying will be immediate like this first quarter or second quarter, it will be a progression in terms of that provision and the quality of it will become apparent as time goes on, is available to every kenyan just by registering.
Healthcare Needs and Services
And that will address 80% of our healthcare needs. If you look at generally population health it's only around 5% who consume high end tertiary care. Majority of the people don't need expensive tertiary care because you will realize, even looking at yourself and your life, when was the last time you were admitted and you needed dialysis or you needed surgery or you needed, you will realize majority of Kenyans would say no, they can't even, they have never needed those things.
Tertiary Care Accessibility
So our consumption is usually it's around 5% of the population who will need very highly specialized services. The second thing that I would address or what would you like to change for me? I would like the courts to allow us to implement the laws as we had designed and more importantly to see that we become a little bit more patriotic and stop this assumption that we'll always be the ones who are earning a lot and we will always be the ones who will be deducted.
Systemic Assumptions
Gross 2.75% this assumption is what some people need to just get out of their mind that anytime anything can change in this life and paying out of pocket is not sustainable. And someone mentioned and say I can't sustain dialysis for a month. That's the reality. For almost 99% of Kenyans, paying a million plus annually is nothing, an easy walk.
Exploring Payment Models
So prepayment is the best method in terms of getting that debate. I'm not sure of whether health is public good or it is a private good. There are those who would say it's a public good. There are those who would say it's a private good and it is understandable. We can't all agree into one thing, but Covid has shown us that health can be of public interest when the time comes.
Public Interest in Health during Crises
When the whole world came to a standstill. It was a disease. So you could have easily said it's your own problem and it none of our business. But it became our business in as much as it was from another country. Not even something that has started locally. On the issue of the input of KMA, I think my president, we will be here nine months from now and we will see the input from KMA at the board level and we will be discussing how far so far were in terms of that input and the difference it will make, which we dont doubt.
Anticipating Future Contributions
But its not that KeMA needed to be at the board level for it to contribute because these laws and everything was done when there was no event, board regulations were done when there was two or three members at the board level. So I don't believe in you can only contribute to something when you are a board member, you can contribute even when you are outside.
Inclusivity in Input and Contribution
So the issue of saying it's not us, there was the option of saying this was not us, we don't want to be appointed. Please look for another association to sit on that seat. That was also something that you could easily have taken. I'm happy Kush has spoken a lot and actually he has made my work much easier.
Healthcare Models and Global Comparisons
So Kush has explained the different models and this is what we need to understand that there's no one size fits all. UK does its tax system, NHS. If you ask the people who live there, patients, individuals. I know kenyan doctors who work in NHS in the UK, but come to Kenya for treatment when they need major surgery and when they need surgeries and such, when you ask them, they will tell you that system is bullshit.
Critiques of the UK's Healthcare System
Sorry, my french, but there are people who look up to that system and say, oh, it's tax funded, it's good. So that tells you there's no perfect system and there's no perfect financing mechanism. Then you talked about Netherlands Netherland insurance is mandatory, same as Shah.
Mandatory Insurance Systems
But what you need to realize is what we are looking at. What is our yield? How much are we collecting? Are we able to push that limit? Yes. Increase the rate from 2.75%, maybe to 10%. What will that give us? It will give us more money.
Considerations on Tax Increases
So are we able now to increase the benefits and the tariffs? Yes. Are we able to increase the caesarean rate? Yes. It all depends on how much more are people willing to contribute or how. How much more are we going to get from the tax fund.
Balancing Funding Sources
So for us, we have done the mixed model contribution plus tax is just to lessen the burden on individual contribution, but have something extra, at least from tax, to balance it. Just allowing it one source of funding was very difficult. Of course, the US has moved the private insurance.
Global Health System Comparisons
Ask around anywhere in the world. You will be told the us system is the worst because it is what my friend Eboso is advocating for, that health is a private good. Let everyone deal with their problems whether they like it or not. But unfortunately, despite that, the US spends the highest amount of money per capita compared to the Scandinavians and the other OECD countries.
Risks of Private Health Systems
So you then realize that privatization without government intervention will just kill the health sector fully and it will be very unsustainable and very catastrophic for majority of the people, even in the US. If you look around and read around, look for that documentary called Ceco, you will see how siko s I c k o.
Challenges of Privatised Health Systems
You will see how bad that system is of where you say this is private good, let everyone pay and then let everyone take care of themselves. Finally, the issue of Robin Hood or the rich should pay less. That is now, you know, another debatable issue.
Equity in Healthcare Funding
So if the rich pays less or pays less rate, then the poor pays more. So who is funding who and who is benefiting more than the other? So those are for me, as I have said, is the debates now that need societal debates, social hole, where we have this discussion and discuss what kind of contribution and whether something is public good or private good and how do we handle the financing mechanisms.
Next Steps and Future Conversations
I think I have touched if I forgotten anything, we will have another session as usual. But this time around I am sure we will not be discussing the basics. We will be now delving into other issues. On the issue of transition, yes, we have faced challenges.
Challenges in Transitioning Healthcare Systems
The challenges we have faced is mainly the system and we have delayed in communication to the providers because generally it's providers who and it's all because of the mistrust that they have had with any. We all know our system does not treat patients, it's hospitals and healthcare workers.
Mistrust in Provider Communication
But because of that lack of mistrust between NHIF that has built up over the years, that's where now there was a small challenge in terms of the communication, reaching and releasing that communication as early as possible, that if you have a challenge with the system, please use manual claim processing so that we patients get services as expected.
Overcoming Access Challenges
So yes, I'm not dismissing that there were hiccups, there were many people who had difficulties in accessing services. And it's not that it's an easy thing on our end to say, it's a small matter. No, nothing is further from the truth.
Monitoring Transition Processes
So yes, we are all warning up. We are not saying, and we are not burying our head in the sun to say everything was smooth, far from it. But we hope to complete this transition by the end of next week. We will have finalized and every facility would have been onboarded because I was looking at the dashboard as late as right now while we are discussing this issue to see how is the consumption, how is the logins from the providers, and I can assure you majority of the facilities, total providers enrolled is around 6900.
Current Enrollment and Future Goals
Facilities have already been onboarded. So we will continue monitoring to see that we transition everyone as much as possible. And I just want to reassure providers that we will make sure even the old claim system, e claims system that was closed, we will open it up and conclude that process once we fully take over and recruit new staff.
Closing Acknowledgment
Thank you very much. Thank you, doctor Abdi, thank you for giving us your time tonight. Just to clarify on the questions that you might have, we wish you and your team all the best, especially during this transition period, as it's mostly the patients that are affected and they usually need services to go on during this time.
Final Thoughts on Transition Challenges
But I just wanted also to end with. You'd say that the hiccups are also usual, but it will also be remiss. Not to mention that we usually use these. The road to hell is paved with good intentions. So however good they might be, we need to look at the transition.
Future Planning Discussions
You'd also recommended that by. I think we can hold another one by November 2024, which I'll follow up keenly that Doctor Mbitti. So just so that we can just put you to task, especially since you've said the system will be fully operational by November 2024.
Conclusion and Acknowledgments
And another thing just before we end, I know you'd say that about the. Mostly about being it employee based, but NTSA police or machine. Now you come, you and your team, to Isana, especially getting contributions from this sector, especially since the informal sector mostly. But thank you for your time and thank you all for tuning in and listening.
Engaging with Audiences on Healthcare Issues
Hope some of your questions have been answered. The next time we hold, we'll try to, just try to keep it short of be more specific with the questions, but it's a learning curve that we're starting with right now. So hopefully we'll have a better, more fruitful discussion next time where we'll have more questions, especially from our listeners.
Conclusion and Goodbye
Thank you all and have a good night. So thanks again. No smoo, I appreciate you here. You know, not everyone takes three, 4 hours late into the night to have this conversation. We'll definitely have a follow up, like Nigel has said. Thank you, everyone.